WASHINGTON — The U.S. Department of Veterans Affairs is processing claims at the fastest rate […]
Category: medical
Governor Roy Cooper Comments on Judge Reinstating 20-Week Abortion Ban
Raleigh Aug 17, 2022 Today, Governor Roy Cooper issued the following statement in response to […]
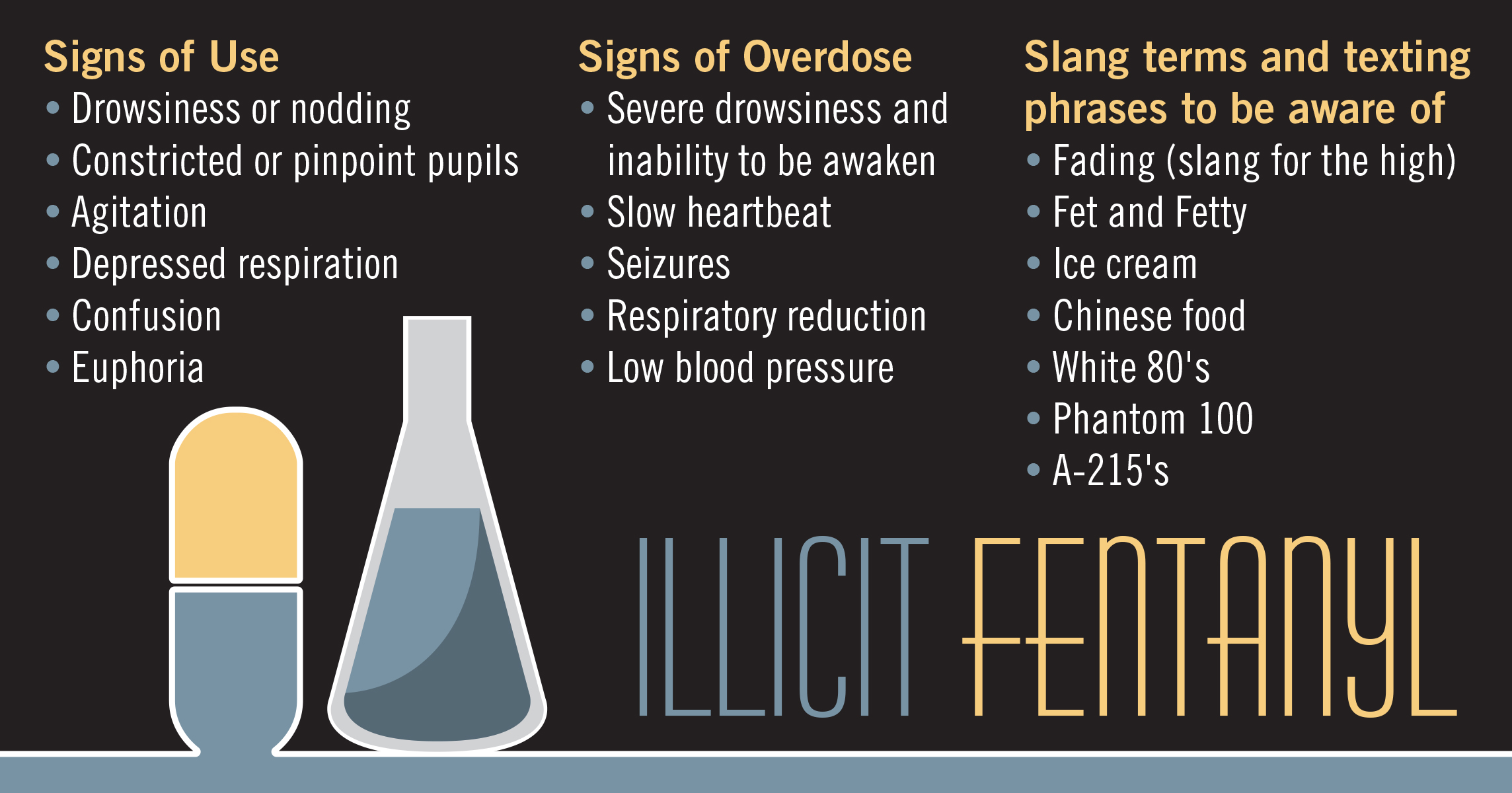
Fentanyl in NC: An epidemic within the opioid epidemic
By Joe Killian – 8/15/2022 NC Policy Watch A year ago this month, Barb Walsh […]
Winterville woman charged with seven counts of Insurance Fraud
RALEIGH Jul 29, 2022 North Carolina Insurance Commissioner Mike Causey today announced the arrest of […]
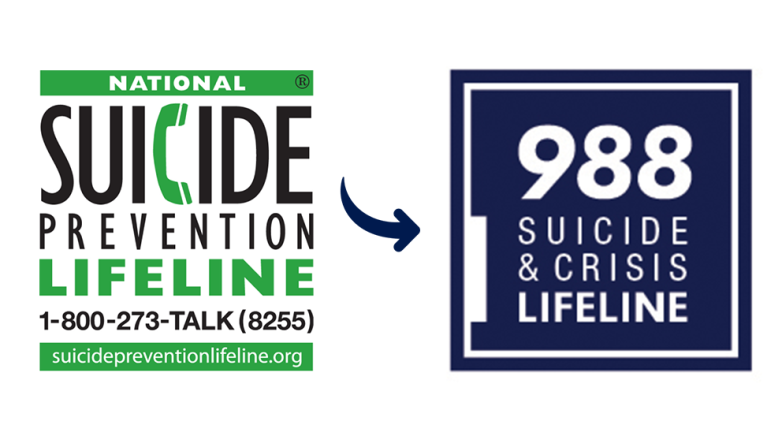
The Lifeline and 988
988 has been designated as the new three-digit dialing code that will route callers to […]
NCDHHS Again Expands Eligibility for Monkeypox Vaccination, Encourages Steps to Reduce Spread
“Get Checked. Get Tested. Get Protected.” Raleigh Jul 25, 2022 The North Carolina Department of […]
Hampered by opposition from doctors’ groups, nurse practitioners want to change state law to give them more freedom to treat patients
By Lynn Bonner – 4/7/2022 NC POLICY WATCH Michelle Skipper has a doctorate in nursing practice and […]
Rural healthcare providers feel the pain of North Carolina’s Medicaid gap
By Lauren Ketwitz – 3/22/2022 NC POLICY WATCH On her morning commute to work, Dr. Laura […]